Quiz-summary
0 of 6 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to pass the previous Module's quiz in order to start this quiz:
Results
Results
0 of 6 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- Answered
- Review
-
Question 1 of 6
1. Question
 Situation
SituationAt the consultation, Lynne’s haematologist explained that given her age, the optimum treatment would be induction treatment followed by high-dose therapy and autologous stem cell transplantation (ASCT). There were no clinical trials available in the area Lynne lived in. She had four other siblings so the possibility of an allogeneic stem cell transplant was also proposed.
However, Lynne was extremely reluctant to have a transplant of any sort because of her family circumstances and her worries about child-care. She had major concerns about the potential side-effects of high-dose therapy, the length of the recovery period post-transplant and the risks associated with both autologous but especially allogeneic transplants. She was also anxious about the need to travel to the nearest transplant centre 40 miles from home.
The haematologist explained that for someone of her age and general fitness, high-dose therapy and an autologous stem cell transplant followed possibly by a reduced-intensity allogeneic stem cell transplant would potentially offer the best chances of longer control of the myeloma. He explained that there were side-effects issues to consider but these could be prevented or managed effectively.
The haematology nurse specialist added there were other measures that could be taken to aid recovery and she would look into the types of support available to help with travel. She suggested Lynne should take time to talk to her family and friends about the various treatment options and arrangements for child-care.
A few days later Lynne called the nurse specialist to say she had carefully considered her options and at this stage, did not want to have a transplant.
Q1: Based on the above case, what treatment would you recommend for this newly diagnosed 39 year old patient?
CorrectIncorrect -
Question 2 of 6
2. Question
 Situation
SituationLynne was started on CTD and put on monthly bisphosphonate infusions of Zometa® in July 2011. Her paraprotein level at the end of cycle one was 68. However, she was also severely neutropenic (0.3 x 109g/L) which was attributed to the cyclophosphamide.
For cycle two and three, cyclophosphamide was reduced to 250mg but Lynne’s paraprotein reading at this point was 72 indicating that she was refractory (failure to achieve at least minimal response) to CTD. Her neutrophil count was 0.2 x 109/L and she also reported bouts of dizziness. On examination, she was found to be bradycardic (45-50/min), a recognised side-effect of thalidomide.
Q2: What would you do now?
CorrectIncorrect -
Question 3 of 6
3. Question
 Situation
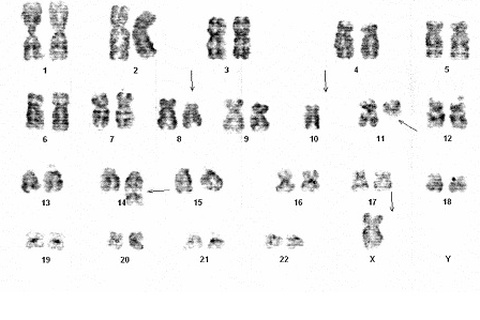
SituationConventional karyotyping revealed several abnormalities (see Figure 1) and fluorescence in situ hybridisation (FISH) analysis showed that Lynne was carrying a t(11:14) translocation, putting her into the “low risk” category.
In theory, Lynne should have benefited from CTD as there is evidence that patients with a favourable cytogenetic profile benefit more from thalidomide-based induction treatment in terms of improved progression-free survival (PFS) and overall survival (OS) than those with an adverse cytogenetic profile [3]. Therefore, it was surprising she was refractory to CTD.
Figure 1 shows karyotype analysis for Lynne showing several abnormalities as depicted by the arrows.
Lynne was visibly upset on hearing she had not responded well to her initial treatment. Her haematologist explained that other drugs were available and these should be tried although it would mean trips to the hospital twice a week.
Lynne started Velcade and dexamethasone treatment in August 2011. She received subcutaneous Velcade on days 1, 4, 8 and 11 of a 21 day cycle and 20mg dexamethasone on each day of Velcade and the day after. Cyclophosphamide was included at the start of cycle 3 once her neutrophil counts had recovered sufficiently and she received once weekly subcutaneous Velcade from then on.
After four cycles, Lynne had not responded well enough to CVD to warrant continued treatment. She achieved stable disease (paraprotein reading of 47) although her last reading showed a small rise again. She also developed grade 1 peripheral neuropathy and her neutrophil counts had dropped again (0.6 x 109/L).
Her haematologist suggested she reconsider high-dose therapy and stem cell transplantation because she had not responded well to any treatment so far and her options were narrowing. The pros and cons of both an autologous and allogeneic stem cell transplantation were repeated at length and Lynne was strongly advised to seriously consider an autologous transplant as the next option.
The nurse specialist spent the afternoon with Lynne going through the procedure and the practicalities of coping and recovering from an autograft. She asked whether Lynne’s siblings would agree to be tested as possible donor matches so that an allograft could be another option in the future.
After much thought and discussion with her family and close friends, she agreed only to have an autograft as a last resort if further drug treatment failed. She knows that Revlimid is the next approved treatment and wants to try this.
All her siblings agreed to be tested and one of her sisters was found to be a suitable donor match.
Q3: What would you do now?
CorrectIncorrect -
Question 4 of 6
4. Question
 Situation
SituationRevlimid was started at a lower dose of 15mg/day on Days 1 – 21 of repeated 28-day cycles as Lynne’s neutrophil counts were so low. She also received dexamethasone at 40mg initially on days 1 – 4, 8 – 11 and 15 – 18 with the aim reducing disease as rapidly as possible.
Lynne did not tolerate Revlimid well, she became very fatigued and her nosebleeds returned. Blood tests after the first cycle showed a neutrophil count of 0.4 x 109/L; haemoglobin level of 8.4g/dL and a platelet count of 42 x 109/L. Her paraprotein reading was 40.
She received blood and platelet transfusions.
Q4: What would you do now?
CorrectIncorrect -
Question 5 of 6
5. Question
 Situation
SituationLynne was asked to reconsider the possibility of an autologous transplant. Having not responded to any of the currently approved treatments, together with the fact that there were no clinical trials being conducted locally, she was told that her options were narrowing considerably: it would be in her best interest to prepare at least for a stem cell harvest.
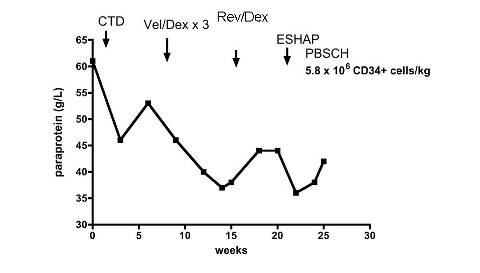
After due deliberation and discussion with her nurse and family, Lynne eventually agreed to begin preparation for stem cell harvest. She received ESHAP over a period of five days followed by GCSF for nine days before stem cells were collected on day 15. At the first attempt, 5.8 x 106 CD34+ cells/kg were harvested and stored.
ESHAP treatment produced a small salvage effect reducing the paraprotein levels by 18%. However, this did not last long and within three weeks, they started to rise again.
Q5: What would you do next?
CorrectIncorrect -
Question 6 of 6
6. Question
 Situation
SituationLynne underwent high-dose therapy and ASCT in Jan 2012 (27 weeks after diagnosis). She developed grade 3/4 mucositis, diarrhoea and then hypokalaemia-induced diabetes insipidus resulting in polyuria and polydipsia.
Neutrophil engraftment was apparent on day +12 and she was discharged from hospital on day +33.
Lynne achieved VGPR with high-dose therapy and ASCT. A bone marrow biopsy four months post-transplant showed 3% plasma cell content. She remains in remission, is recovering well from her transplant and is enjoying time with her children again.
Figure 2 shows a profile of Lynne’s treatment response
Q6: What would you do next?
CorrectIncorrect